Understanding and Preventing Your Low Back Pain Part 3 Disc Disorders
About 80% of Americans suffer debilitating low back pain at some point in their life. This fact is staggering, yet it doesn’t have to be this common. The key to staying out of this group of low back pain sufferers comes down to one word: Prevention. If I had to choose one common problem amongst all low back pain sufferers, it would be a bad low back position during common activities such as brushing your teeth, bending over, picking up a small child, exercising and sitting.
The lumbar spine, which is the lower part of the spine, is meant to have a natural curve to it that displaces the forces of gravity, weight, etc. evenly and minimally. When this natural curve is straightened or reduced, the forces on the discs, muscles, and ligaments of the low back are significantly increased. For example, sitting without maintaining the natural curve increases the forces on those structures by 30-40%!
There are many conditions that can be covered under the umbrella of low back pain, but in this article, we will cover the following conditions for the sake of this informational handout. The keys to prevention of low back pain are as follows:
• Understand your symptoms and risk factors
• Body Preparation and Positioning
• Proper Activities of Daily Living
• Corrective Exercises
• Treatment Considerations
Common Low Back Conditions
Lumbar Disc Disorders

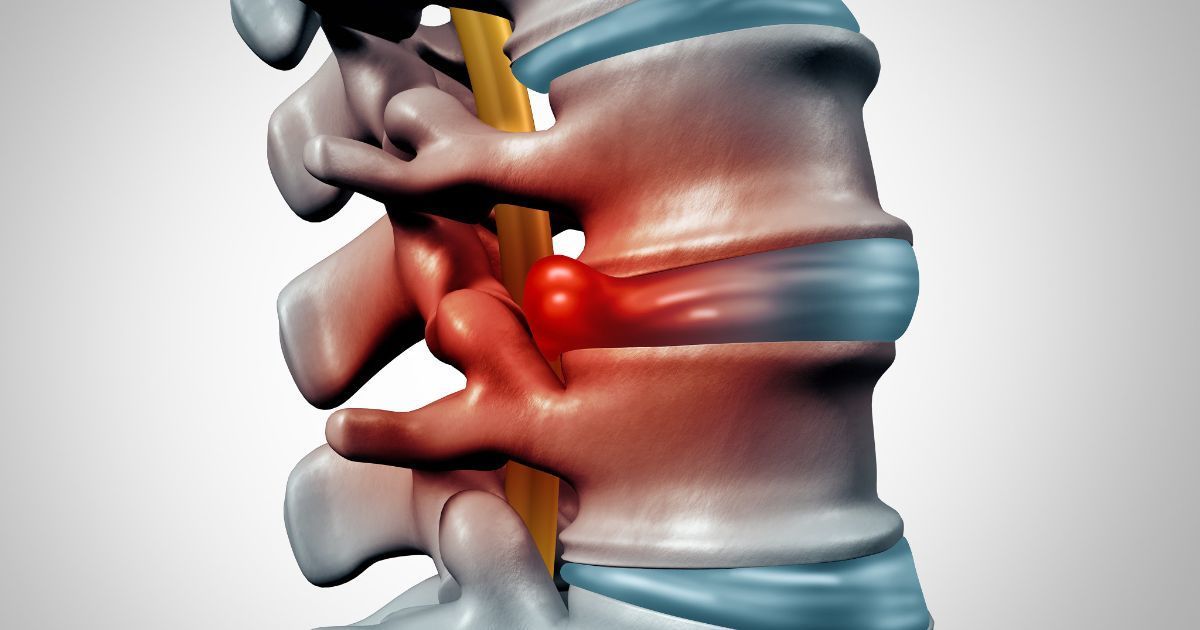
The lumbar spine is made up of five bone segments called vertebrae. In between each vertebra are flexible intervertebral lumbar discs, which act as shock absorbers for the spine. The intervertebral discs are composed of two components, a tough outer ring of fibrous tissue called the annulus fibrosis, and a jelly-like center inside the annulus fibrosis called the nucleus pulposus. The structure is then held together by ligaments on the front and the back of the vertebrae. Additional support is provided by the muscles of the trunk.
In most cases, lumbar disc disease is the result of a normal ageing process called disc degeneration, which causes structural changes in the normal disc. As we age, the disc begins to lose fluid and become dried out causing the disc to compress. This may lead to the breakdown and degeneration of tough outer ring of the disc (annulus fibrosis), allowing the inner core (nucleus pulposus) to bulge out. This is considered a bulging disc. This puts pressure on the outer ring of the disc, which may cause low back pain. As further degeneration of the disc continues, or with continued stress on the lumbar spine, the inner jelly-like core may rupture out from the outer ring, causing a ruptured or herniated disk. Once the inner nucleus herniates through the outer ring, pain in the lower back may improve.
However, the fragmented disc material can inflame or put pressure on the spinal nerves leading to an increase in sciatic leg pain, weakness, numbness, or changes in sensation in one or both legs. Most disc herniations occur at the lower lumbar spine at L4-L5 and L5-S1 levels. Occasionally, severe trauma can cause a normal disc to herniate or may cause an already herniated disk to worsen.
Risk Factors of Lumbar Disc Disorders
● Age and Gender - the highest incidence in men between the ages of 30 and 50.
● Obesity - being overweight puts added stress on lumbar discs.
● Sedentary lifestyle - lack of exercise and poor core body strength.
● Smoking - Smoking decreases oxygen supply to the discs causing more rapid degeneration.
● Improper lifting - using your back muscles instead of your legs to lift heavy objects. Twisting while lifting
● Posture - hyperlordotic lumbar curvature, anterior pelvic tilt (lower cross syndrome).
● Repetitive activities that strain your spine - jobs that require constant lifting, pulling, bending, or twisting.
● Frequent driving - staying seated for long periods, and the vibration from the car can put pressure on your discs.
History and Symptoms of Lumbar Disc Disorders

Lumbar disc disorders may include one or a combination of the following symptoms:
• Intermittent or constant lower back pain and pain in the buttock,
• leg and foot pain, numbness or a tingling sensation in the leg and foot,
• Weakness in the leg and foot
• Decreased reflexes in the knee or ankle
• Changes in bowel or bladder function.
The symptoms will vary depending on if and where the disc has herniated, and what spinal nerve root is affected. Leg pain is usually greater than low back pain with disc herniations and nerve root involvement. However, if there are only annular tears without herniation, the pain will be localized to the low back and buttock. The onset of pain can be sudden or gradual after an injury. Pain may follow heavy lifting, twisting, or straining activities or repetitive stress trauma. However, patients may not recall a prior injury or a precise time the condition began because it is often preceded by frequent episodes of less severe low back pain that usually resolved. Pain is usually characterized by sharp, shooting, or electrical pain that may be aggravated by movement, changing positions, sneezing, coughing, or prolonged sitting and standing. The pain is usually relieved with rest and a recumbent position.
Treatment of Lumbar Disc Disorders
Conservative care should be your first course of treatment to manage lumbar disc disorders, but treatment will depend on the clinical presentation, your age, overall health, and tolerance to therapies. With disc herniation, the first few days of care will focus on centralizing (reducing) leg pain, decreasing inflammation, and preventing further neurological loss by decompressing nerve root impingement and reducing the disc herniation. Osseous mobilization and manipulation and soft tissue therapy may be administered as tolerated. Home care will consist of pain-relief repetitive positional exercises and lumbar stabilization exercises. We will also educate you on ways to protect your lower back, positions to avoid, and how to manage activity. In most cases, bed rest will not be recommended as the sooner you are up and moving, the better the prognosis. Once pain and inflammation have decreased, we will continue working on lumbar stabilization and progress into proprioceptive training. We will evaluate muscle imbalances using posture and movement patterns with the goal of restoring good biomechanics and core body strength. Your home care will emphasize the progression of stabilization protocols and corrective exercises. If you fail to respond to conservative treatment, or in cases of severe neurological loss, a referral for a surgical consultation will be recommended.
Also, a recent study demonstrated that folks that have chiropractors as part of their low back healthcare team are 64% less likely to take opioids. In this study, there was strong support for chiropractic care, helping to decrease pain, increase mobility and ultimately increase function. Who wouldn’t want a drug free solution to these problems?


